What Does Lymphostasis Look Like? Understanding the Appearance and Stages
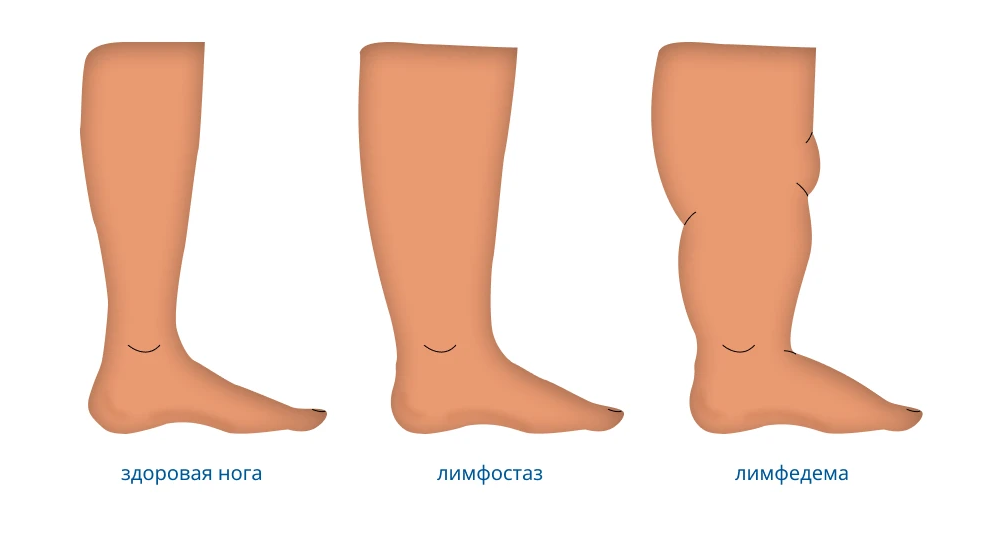
Lymphostasis, also known as lymphedema, is a chronic condition that occurs when the lymphatic system doesn’t properly drain lymph fluid, leading to swelling, typically in an arm or leg. Understanding what does lymphostasis look like is crucial for early recognition and management. This article will detail the visual characteristics of lymphostasis across its various stages and affected areas.

Early Signs of Lymphostasis pictures
In its initial stages (picture 1), what lymphostasis looks like can be subtle and easily overlooked. Early signs may include:
- Mild Swelling: A feeling of heaviness or fullness in the affected limb. The swelling might be intermittent, worsening during the day and improving overnight.
- Pitting Edema: Pressing on the swollen area with a finger may leave a temporary indentation or pit. However, in later stages, the tissue can become more fibrotic, and pitting may be less apparent.
- Tightness of Skin: The skin on the affected limb may feel tight or firm.
- Decreased Flexibility: Difficulty moving joints in the swollen limb.
- Aching or Discomfort: A dull ache or discomfort in the affected area.
- Changes in Skin Texture: The skin may start to feel slightly different, perhaps thicker or warmer.
Visually, in these early phases, what lymphostasis looks like might just be a slight increase in the size of the limb compared to the unaffected side.
Progressive Stages of Lymphostasis photos
As lymphostasis (photo 2) progresses, the visual characteristics become more pronounced. Understanding what lymphostasis looks like in its later stages is important for recognizing the need for more intensive treatment.
- Increased Swelling: The swelling becomes more persistent and significant. The affected limb can become noticeably larger and heavier.
- Non-Pitting Edema: The tissue becomes more fibrotic (hardened and thickened), and pressing on the swollen area no longer leaves a pit. This is a key indicator of more advanced lymphostasis and what advanced lymphostasis looks like.
- Skin Changes: The skin may undergo several changes in texture and appearance:
- Thickening (Fibrosis): The skin and underlying tissues become thick and firm.
- Hardening (Sclerosis): The skin can feel hard and leathery.
- Papillomatosis: The development of small, wart-like growths on the skin surface, indicating severe, long-standing lymphostasis and what severe lymphostasis looks like.
- Hyperkeratosis: Thickening of the outer layer of the skin, making it rough and scaly.
- Increased Skin Folds: Deep creases or folds may develop in the swollen limb.
- Color Changes: In some cases, the skin may develop a brownish discoloration (hyperpigmentation).
- Increased Risk of Infections (Cellulitis): Repeated infections can cause redness, warmth, pain, and further changes in the skin’s appearance.
- Shape Deformity: The shape of the affected limb can become distorted due to the excessive swelling and tissue changes. This is a significant aspect of what chronic lymphostasis looks like.
- Limited Mobility: The increased size and stiffness of the limb can severely restrict movement and functionality.

Lymphostasis images in Body
While the arms and legs are most commonly affected, lymphostasis (image 3) can occur in other parts of the body. What lymphostasis looks like can vary depending on the location:
- Arm Lymphostasis: Typically occurs after breast cancer treatment involving lymph node removal or radiation. What arm lymphostasis looks like is swelling in the arm, hand, and sometimes the fingers. The arm may feel heavy and tight, and there might be visible differences in size compared to the other arm.
- Leg Lymphostasis: Can result from cancer treatment (e.g., for pelvic cancers, melanoma), vascular issues, or congenital abnormalities. What leg lymphostasis looks like is swelling in the thigh, calf, ankle, and foot. The leg may feel cumbersome, and skin changes can be prominent.
- Head and Neck Lymphostasis: Can occur after surgery or radiation for head and neck cancers. What head and neck lymphostasis looks like includes swelling in the face, neck, and sometimes the tongue or throat. This can cause discomfort and functional issues.
- Genital Lymphostasis: Can be caused by surgery, radiation, or infections. What genital lymphostasis looks like is swelling in the external genitalia, which can be significant and distressing.
- Truncal Lymphostasis: Swelling in the chest, back, or abdomen, often associated with breast cancer treatment. What truncal lymphostasis looks like is a less common presentation but can cause discomfort and tightness in the affected area.

Causes and Risk Factors of Lymphostasis
Understanding the causes can help in identifying individuals at risk and recognizing what might lead to lymphostasis (pics 4):
- Primary Lymphostasis: A rare condition caused by congenital abnormalities in the lymphatic system. The onset may occur at birth (congenital lymphedema), during puberty (lymphedema praecox), or later in adulthood (lymphedema tarda). The appearance depends on the severity of the lymphatic dysfunction.
- Secondary Lymphostasis: More common and results from damage to or blockage of the lymphatic system. Common causes include:
- Cancer Treatment: Surgery involving lymph node removal (e.g., mastectomy, lymph node dissection) and radiation therapy are major risk factors.
- Infections: Recurrent infections, particularly cellulitis, can damage lymphatic vessels. Filariasis, a parasitic infection, is a leading cause of secondary lymphedema worldwide but is less common in some regions.
- Trauma: Significant injury to the lymphatic system.
- Vascular Conditions: Certain vascular diseases can impair lymphatic drainage.
- Obesity: Severe obesity is associated with an increased risk of lymphedema.
- Tumors: Tumors can directly obstruct lymphatic vessels or nodes.

Diagnosis of Lymphostasis Based on Appearance and Other Factors
Diagnosis of lymphostasis often relies on a thorough clinical evaluation, including a detailed medical history and physical examination. Recognizing what the swelling looks like and considering risk factors are key. Diagnostic tools may include:
- Physical Examination: Assessing the swelling, skin changes, and presence or absence of pitting edema. Measuring the circumference of the affected and unaffected limbs to quantify the difference in size.
- Medical History: Reviewing the patient’s history of cancer treatment, infections, trauma, and other relevant conditions.
- Lymphoscintigraphy: An imaging technique that tracks the flow of a radioactive tracer injected into the lymphatic system to identify blockages or abnormalities.
- Magnetic Resonance Lymphangiography (MRL): A more detailed imaging technique that provides high-resolution images of the lymphatic vessels.
- Doppler Ultrasound: To rule out venous insufficiency as a cause of swelling.
- Bioimpedance Spectroscopy (BIS): A non-invasive method to measure fluid levels in the tissues.

Management and Treatment of Lymphostasis and Its Appearance
Management of lymphostasis aims to reduce swelling, control pain, prevent infections, and improve the function and appearance of the affected limb. Understanding how to manage lymphostasis and its visual impact is crucial for patients.
- Complete Decongestive Therapy (CDT): A multi-component therapy that is the gold standard for lymphedema management. It includes:
- Manual Lymphatic Drainage (MLD): A gentle massage technique to help move lymph fluid out of the swollen limb.
- Compression Therapy: Using bandages and compression garments to support the limb and prevent fluid buildup.
- Exercise Therapy: Specific exercises to promote lymphatic drainage and improve limb function.
- Skin Care: Maintaining good skin hygiene to prevent infections.
- Compression Garments: Custom-fitted garments worn daily to maintain the reduction in swelling achieved through CDT.
- Pneumatic Compression Devices: Inflatable sleeves that apply sequential pressure to the limb to help move fluid.
- Surgery: In some cases, surgical options may be considered, such as lymphovenous bypass or lymph node transfer, to improve lymphatic drainage. Liposuction can be used to reduce the volume of fatty tissue in chronic lymphedema.
- Medications: There are currently no medications to cure lymphedema, but antibiotics are used to treat infections. Research into pharmacological treatments is ongoing.
Recognizing what lymphostasis looks like in its various stages and locations is essential for early diagnosis and effective management. From subtle swelling and skin tightness in the early phases to significant limb enlargement and skin changes in more advanced stages, the visual characteristics of lymphostasis are key indicators of the condition. Understanding the causes, risk factors, and available treatment options empowers individuals and healthcare providers to address lymphostasis proactively, improving the quality of life for those affected.