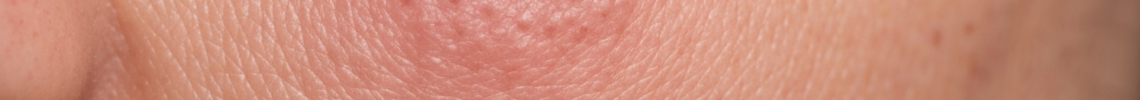
When trying to understand what Actinic Keratosis looks like, it’s crucial to observe the specific visual and tactile characteristics of these sun-induced lesions. These pre-cancerous patches, also known as solar keratosis, present with distinct features that distinguish them on the skin, often in areas of significant sun exposure.
Actinic keratosis Symptoms Pictures
Actinic keratosis, commonly abbreviated as AK, manifests with several characteristic visual symptoms that are vital for early identification. These sun-damaged skin lesions primarily appear as rough, scaly patches or bumps on the skin. The texture is frequently described as feeling like sandpaper when touched, an important tactile symptom that often precedes visible changes. The coloration of actinic keratosis lesions can vary significantly, ranging from flesh-toned, making them difficult to spot without close inspection, to distinct shades of pink, red, light brown, or even dark brown, especially in individuals with a history of extensive sun exposure. Sometimes, a combination of these colors might be present within a single lesion or across multiple actinic keratoses on a patient’s skin. The size of these rough patches can range from a pinhead to more than a quarter of an inch in diameter, often growing slowly over time. They typically develop in areas frequently exposed to the sun’s ultraviolet (UV) radiation, including the face, scalp (especially in bald individuals), ears, lips, neck, forearms, and the back of the hands. Actinic keratosis symptoms can also include a feeling of tenderness, itching, or a burning sensation when the lesions are touched or irritated, though many individuals experience no discomfort at all, making visual and tactile inspection the primary method of detection. The edges of an actinic keratosis lesion can be well-defined or blend subtly into the surrounding sun-damaged skin, which often shows other signs of photoaging, such as wrinkles, hyperpigmentation, and telangiectasias (spider veins). In some cases, actinic keratosis may present as a thickened, horny growth, a condition known as cutaneous horn, which appears as a conical or cylindrical projection from the skin surface, indicative of a more advanced or hyperkeratotic actinic keratosis. This severe form requires immediate attention from a dermatologist due to an increased risk of progression to squamous cell carcinoma. The surface of these sun spots can also sometimes be covered with a yellowish or whitish scale that may flake off, revealing a raw or slightly reddened base. This persistent scaling and crusting are key visual identifiers of many actinic keratosis lesions.
Detailed visual characteristics of actinic keratosis symptoms include:
First, the *rough texture*: These are palpable rough patches, often feeling like coarse sandpaper or a small, hardened scab that never fully heals. This texture is a hallmark of actinic keratosis lesions and is often the first symptom noticed by individuals or their dermatologists during a skin examination.
Second, *variable coloration*: Actinic keratosis can present in a spectrum of colors. This includes subtle, skin-colored patches that are hard to see but easy to feel, as well as more pronounced pink or reddish spots due to increased blood flow or inflammation. Brown or dark spots may also indicate pigmented actinic keratosis, which can sometimes be confused with lentigo maligna or other pigmented lesions, necessitating a thorough dermatological assessment for accurate diagnosis of the skin condition.
Third, *scaly or crusty surface*: Many actinic keratoses are covered by a dry, adherent scale that can be white, yellow, or brownish. This scale can be thick and tenacious or fine and flaky, contributing to the rough feel. Sometimes, an actinic keratosis might appear as a persistent crust that reforms even if picked or scratched off, indicating ongoing cellular changes in the affected skin.
Fourth, *sun-exposed distribution*: The vast majority of actinic keratosis lesions are found on areas of chronic sun exposure. This includes the face, especially the forehead and nose, the ears, the balding scalp, the back of the hands, forearms, and the V of the neck. This characteristic distribution is a crucial diagnostic clue for healthcare providers evaluating suspicious skin lesions for signs of sun damage and potential skin cancer risk.
Fifth, *variable size and shape*: Actinic keratoses can be small, barely noticeable dots, or grow into larger, irregular patches. They can be round, oval, or have an amorphous, ill-defined shape, sometimes merging with adjacent lesions to form larger areas of field cancerization, where multiple pre-cancerous cells are present within a larger area of sun-damaged skin. The borders can be distinct or poorly demarcated, blending into surrounding healthy-looking skin.
Sixth, *occasional symptoms of discomfort*: While many actinic keratosis lesions are asymptomatic, some can be itchy, tender to touch, or cause a mild stinging or burning sensation. These symptoms, though not universal, can prompt individuals to seek medical attention and reveal underlying actinic damage.
Seventh, *thickened or warty appearance*: In some cases, actinic keratosis can evolve into a hypertrophic form, appearing as a significantly raised, thickened, or warty lesion. These elevated actinic keratosis lesions have a higher potential for progression to invasive squamous cell carcinoma and warrant prompt evaluation by a skin cancer specialist. They often have a very prominent, hard, and rough surface.
Signs of Actinic keratosis Pictures
The observable signs of actinic keratosis provide critical information for diagnosis and risk assessment, particularly when viewed by a dermatologist during a comprehensive skin check. These pre-cancerous skin lesions are fundamentally a manifestation of chronic sun damage, and their appearance often correlates with the degree of UV exposure. One of the most consistent signs is the presence of a palpable, rough patch on sun-exposed skin. This tactile sensation is often more reliable than visual detection in the early stages of actinic keratosis. Visually, these patches are characterized by a persistent scale or crust, which can be fine and whitish or thick and yellow-brown. The underlying skin typically appears erythematous (red) or pigmented. The redness is often a result of inflammation or increased vascularity within the lesion, while pigmentation suggests an accumulation of melanin, particularly in pigmented actinic keratosis. Actinic keratosis can be solitary, but it is common to find multiple lesions, sometimes dozens, scattered across sun-damaged areas, indicating a widespread problem known as field cancerization. The skin surrounding these actinic keratosis lesions often shows other signs of photoaging, such as mottled pigmentation, solar elastosis (yellowish, thickened skin with deep furrows), and telangiectasias, which are dilated small blood vessels visible on the skin surface. These concomitant signs strengthen the diagnosis of actinic keratosis and highlight the extent of underlying sun damage. A crucial sign to monitor is any rapid change in size, shape, color, or texture, or the development of ulceration or bleeding, as these could indicate progression to invasive squamous cell carcinoma, a more serious form of skin cancer. The presence of a firm, indurated base, which means the lesion feels hardened or thickened beneath the surface, is another worrisome sign that necessitates urgent dermatological evaluation and often a biopsy to rule out malignancy. The various morphological types of actinic keratosis also present with distinct signs. For instance, atrophic actinic keratosis appears as a flat, smooth, slightly depressed, and often reddish patch with minimal scaling, while hypertrophic actinic keratosis is significantly raised and thickened with prominent scaling. Pigmented actinic keratosis, as mentioned, mimics other pigmented lesions, making dermatoscopic examination essential for differentiation. Erythematous actinic keratosis is characterized primarily by redness with a fine scale, and it is a very common presentation of sun-damaged skin. The key is that these are persistent signs; an actinic keratosis lesion will not spontaneously resolve and typically remains, or progresses, without intervention.
Key observable signs of actinic keratosis include:
Firstly, *palpable roughness*: The most consistent sign of actinic keratosis is the characteristic rough texture, which can be detected by touch even before the lesion is clearly visible. This sandpaper-like feel is due to abnormal keratinization of the skin cells, a direct result of chronic sun exposure and cellular damage. This tactile sign is crucial for early detection of these sun spots.
Secondly, *erythema or discoloration*: Actinic keratosis lesions frequently present as persistent red or pink patches, often with a fine overlying scale. The redness is indicative of inflammation within the epidermis. In other cases, they may appear as brown or dark spots, known as pigmented actinic keratosis, which can be challenging to differentiate from other pigmented lesions without expert evaluation, such as from a dermatologist or skin cancer specialist.
Thirdly, *adherent scaling or crusting*: A visible sign is the presence of a dry, flaky, or crusty surface that is firmly attached to the lesion. This scale is often white, yellow, or gray and may be difficult to remove without causing a small amount of bleeding. The persistence of this scale is a key diagnostic feature of actinic keratosis lesions.
Fourthly, *telangiectasias (spider veins)*: Frequently, actinic keratosis lesions are surrounded by or contain small, dilated blood vessels visible on the skin surface. These telangiectasias are another indicator of chronic sun damage and photoaging, often co-occurring with actinic keratosis and other forms of sun-damaged skin.
Fifthly, *induration or thickening*: A concerning sign is the development of induration, meaning the lesion feels firm, hardened, or thickened when pressed. This particular sign may suggest a more advanced actinic keratosis or even early invasive squamous cell carcinoma, necessitating urgent biopsy and histopathological examination for precise diagnosis and management.
Sixthly, *field cancerization*: Often, multiple actinic keratosis lesions are present within a broader area of sun-damaged skin, a phenomenon termed field cancerization. This indicates extensive damage to the epidermis, where many cells have undergone pre-cancerous changes, increasing the risk of developing new lesions and invasive skin cancer. This widespread presentation often requires field-directed therapies.
Seventhly, *ulceration or bleeding*: While less common for typical actinic keratosis, any lesion that persistently bleeds, crusts, or develops an open sore (ulceration) without trauma is a significant red flag. These signs are highly suspicious for progression to invasive squamous cell carcinoma and require immediate medical attention for accurate diagnosis and skin cancer treatment.
Eighthly, *rapid growth or tenderness*: An actinic keratosis lesion that exhibits rapid growth, becomes significantly larger over a short period, or develops increasing tenderness or pain, especially when touched, should be promptly evaluated. These changes can signal malignant transformation and necessitate a biopsy.
Early Actinic keratosis Photos
Detecting early actinic keratosis is crucial for effective management and preventing progression to more serious forms of skin cancer. In its initial stages, actinic keratosis can be very subtle and often more easily felt than seen. Early actinic keratosis lesions typically appear as small, slightly rough patches on the skin, often less than 1 centimeter in diameter. Visually, they may be skin-colored or very faintly pink or reddish, blending almost imperceptibly with the surrounding healthy skin. The surface of these early sun spots might have a barely perceptible fine scale, making them feel like a patch of dry skin or a tiny scab that doesn’t heal. They often lack the prominent redness, thickness, or crusting associated with more developed actinic keratoses. Due to their subtle nature, early actinic keratosis can be mistaken for dry skin, eczema, or even age spots (solar lentigines) by an untrained eye. However, a key differentiating factor is the persistent roughness to the touch, which distinguishes them from generally smooth benign lesions. These nascent lesions commonly develop on areas with the highest cumulative sun exposure, such as the forehead, nose, cheeks, temples, ears, and the back of the hands. They are frequently found in individuals over the age of 40, especially those with fair skin, light eyes, and a history of significant sun exposure or sunburns. The evolution of an early actinic keratosis involves a slow process where the abnormal keratinocytes (skin cells) proliferate and accumulate, leading to increased roughness, scaling, and eventual changes in color and thickness. At this early stage, they are entirely confined to the epidermis (the outermost layer of the skin), making them non-invasive and highly amenable to various treatment options that effectively remove the affected skin cells. The recognition of these subtle early signs is paramount for early intervention, which can prevent the potential for malignant transformation into invasive squamous cell carcinoma. Regular self-skin examinations and professional full-body skin checks by a dermatologist are essential for identifying these elusive early actinic keratosis lesions. Early actinic keratosis may also present as a slight, localized patch of altered texture that is only noticeable when skin is stretched taut, revealing a subtle, almost translucent discoloration.
Key visual and tactile cues for early actinic keratosis include:
Firstly, *subtle roughness to touch*: The most consistent and often first sign of an early actinic keratosis is a slight, sandpaper-like texture that is felt when running a finger across the skin. Visually, the area might appear normal or only minimally altered, making the tactile examination critical for detecting these nascent sun-damaged skin lesions.
Secondly, *minimal discoloration*: Early actinic keratosis lesions are frequently flesh-toned or very faintly pink. They lack the pronounced redness or pigmentation of more advanced lesions. This subtle coloration allows them to blend in with the surrounding skin, making them easily overlooked without careful inspection during a skin examination.
Thirdly, *small size*: Typically, early actinic keratosis lesions are quite small, often just a few millimeters in diameter. They can be singular or appear as small, scattered patches across sun-exposed skin, indicating the beginnings of field cancerization due to chronic UV exposure.
Fourthly, *fine, barely visible scale*: A very fine, thin scale might be present on the surface of an early actinic keratosis. This scale is often so delicate that it can be mistaken for normal dryness or flaky skin. Unlike more developed lesions, the scale is not thick or crusty, but rather a subtle indication of abnormal keratinocyte turnover.
Fifthly, *flat or slightly raised appearance*: Most early actinic keratoses are flat or only minimally elevated from the skin surface. They do not have the significant thickness or warty appearance of hypertrophic actinic keratosis, which develops later in the progression of the sun spot. Their lack of significant elevation contributes to their elusive nature.
Sixthly, *persistence*: Unlike transient dry patches or minor skin irritations, an early actinic keratosis lesion will persist for weeks, months, or even years without resolving spontaneously. This chronic nature is a key indicator that a dermatologist should evaluate the lesion, particularly if it’s on a sun-exposed area like the face or scalp.
Seventhly, *absence of significant symptoms*: Early actinic keratosis lesions are often asymptomatic, meaning they do not cause pain, itching, or burning. This lack of discomfort contributes to their late detection, underscoring the importance of proactive skin checks for any new or persistent rough patches on the skin.
Eighthly, *predominant on high sun exposure areas*: Almost exclusively, early actinic keratosis lesions are found on areas of the body that receive the most direct and prolonged sun exposure. This includes the face, especially the forehead and nose, the ears, the balding scalp, and the back of the hands and forearms. This consistent anatomical distribution is a crucial clue for identifying these pre-cancerous lesions.
Skin rash Actinic keratosis Images
While actinic keratosis is typically described as discrete lesions, it can sometimes present in a widespread manner that might resemble or be perceived as a “skin rash,” particularly in cases of severe field cancerization. This widespread manifestation is crucial for understanding the full spectrum of actinic damage. When numerous actinic keratosis lesions develop in close proximity or cover a large anatomical area due to extensive cumulative sun exposure, the overall appearance can mimic a chronic, persistent rash. Instead of isolated bumps, individuals may observe a broad area of skin exhibiting diffuse redness, widespread roughness, and multiple scattered scaly patches. This “rash-like” presentation of actinic keratosis often affects the entire face, the balding scalp, the V of the neck, or the dorsal aspects of the forearms and hands. The skin in these areas will not only feel rough to the touch due to countless small actinic keratoses but will also often appear diffusely mottled with varying shades of red, pink, and brown pigmentation, interspersed with areas of solar elastosis (yellowish, thickened skin). This broad field of sun-damaged skin can be challenging to treat with targeted approaches alone, often necessitating field-directed therapies that treat the entire affected area rather than individual lesions. The distinguishing features from a typical inflammatory skin rash (like eczema or allergic dermatitis) include the persistent, sandpaper-like texture, the chronic nature (it doesn’t typically flare and subside like an allergic reaction), and its exclusive occurrence on sun-exposed areas. Moreover, unlike many rashes, the individual components of this “actinic rash” are often firm or hyperkeratotic to the touch, rather than soft papules or vesicles. The scales associated with this diffuse actinic keratosis “rash” are typically dry and adherent, contrasting with the weeping or oozing scales sometimes seen in eczematous conditions. The background skin often exhibits signs of photoaging, such as deep wrinkles, laxity, and prominent telangiectasias, which are less common with inflammatory rashes. Individuals with a history of outdoor occupations, significant recreational sun exposure, or immunosuppression are particularly prone to developing this extensive form of actinic keratosis, often requiring comprehensive dermatological evaluation and management strategies. Early recognition of this “rash-like” presentation is vital for comprehensive skin cancer prevention, as it indicates a high burden of pre-cancerous cells and an elevated risk of progression to invasive squamous cell carcinoma, demanding a robust approach to skin health and sun protection.
Key characteristics of actinic keratosis presenting as a “skin rash” include:
Firstly, *widespread diffuse redness*: Instead of discrete red spots, a large area of sun-damaged skin may exhibit generalized erythema, giving the appearance of a persistent, reddish rash. This redness is often punctuated by individual rough, scaly patches of actinic keratosis, making the overall field appear inflamed and chronically irritated, particularly on the face, scalp, and forearms.
Secondly, *generalized roughness and scaling*: The entire affected area, not just isolated spots, will feel persistently rough to the touch, akin to sandpaper. This is due to the presence of countless small, often subtle, actinic keratosis lesions that collectively contribute to a diffuse texture change. Fine, dry scales may be present throughout the field, contributing to the “rashy” appearance.
Thirdly, *multiple clustered lesions*: Actinic keratosis often appears in groups or clusters, especially on the forehead, temples, cheeks, and balding scalp. When these clusters are dense and numerous, they can merge visually to create the impression of a widespread eruption or chronic skin rash. This aggregation signifies extensive field cancerization, where a broad area of skin has undergone pre-cancerous changes.
Fourthly, *mottled pigmentation*: The background skin within this “actinic rash” will frequently display irregular or mottled pigmentation, including lighter and darker patches (dyspigmentation), solar lentigines (age spots), and areas of hypopigmentation. This varied coloring is a strong indicator of chronic sun damage, differentiating it from more uniform inflammatory rashes.
Fifthly, *chronic and persistent nature*: Unlike acute rashes that might resolve with treatment or avoidance of triggers, the “actinic keratosis rash” is chronic and persistent, reflecting ongoing epidermal dysplasia. It does not typically clear up on its own and tends to worsen over time without specific dermatological intervention targeting sun-damaged skin and pre-cancerous lesions.
Sixthly, *absence of typical rash features*: While it may look like a rash, it lacks classic features of inflammatory rashes such as pruritus (intense itching) as the primary symptom, blistering, weeping, or significant swelling. The sensation is more typically a persistent roughness, occasional tenderness, or a mild burning, but rarely the intense itch associated with conditions like eczema or contact dermatitis.
Seventhly, *co-occurrence with severe photoaging*: The skin exhibiting this “actinic keratosis rash” often shows other pronounced signs of severe photoaging, including deep wrinkles, significant laxity, and prominent telangiectasias (spider veins). These accompanying signs further confirm the extensive sun damage underlying the “rash” and its etiology as actinic keratosis, rather than an inflammatory dermatosis.
Eighthly, *response to field-directed therapies*: Unlike inflammatory rashes that respond to anti-inflammatory creams, this type of widespread actinic keratosis “rash” responds to field-directed treatments designed to target broad areas of sun-damaged and pre-cancerous skin. This specific treatment response helps distinguish it from other dermatological conditions and confirms its nature as extensive actinic damage.
Actinic keratosis Treatment
Actinic keratosis treatment is essential not only to remove existing lesions but also to reduce the risk of progression to invasive squamous cell carcinoma, a type of skin cancer. The choice of treatment for actinic keratosis depends on several factors, including the number and location of lesions, their size, the patient’s skin type, previous treatments, and overall health. Dermatologists often employ a range of treatment options, broadly categorized into lesion-directed therapies and field-directed therapies. Lesion-directed therapies target individual actinic keratosis spots, while field-directed therapies treat larger areas of sun-damaged skin with multiple visible or subclinical actinic keratosis lesions, addressing the phenomenon of field cancerization.
Detailed treatment options for actinic keratosis include:
Firstly, *Cryotherapy*: This is one of the most common and effective lesion-directed treatments for individual actinic keratosis lesions. It involves applying liquid nitrogen to freeze the lesion, causing the abnormal skin cells to die and eventually slough off. The procedure is quick, typically lasting only a few seconds per lesion. Post-treatment, the area may blister, crust, and then heal over 1-3 weeks, leaving a temporary red or dark spot that usually fades. Cryotherapy is highly effective for single or a few scattered actinic keratosis lesions, particularly on the face, scalp, and hands. It effectively destroys the pre-cancerous cells through extreme cold, prompting the growth of new, healthy skin in its place. The cosmetic outcome is generally excellent, making it a popular choice for superficial actinic keratosis. Mild discomfort during and immediately after the procedure is common, often described as a stinging or burning sensation.
Secondly, *Topical Medications*: These are field-directed therapies applied over a broad area to treat multiple actinic keratosis lesions, including those not yet visible (subclinical). The most common topical treatments include:
1. *Fluorouracil (5-FU) cream*: This chemotherapy cream targets rapidly dividing cells, effectively destroying actinic keratosis cells. Treatment typically lasts 2-4 weeks. Patients often experience significant inflammation, redness, crusting, and erosion in the treated area, which indicates the medication is working. The treated skin will look significantly red and raw before healing, which can take several weeks after discontinuing the cream. It is highly effective in clearing large fields of actinic keratosis, reducing the burden of sun-damaged skin and preventing future skin cancer.
2. *Imiquimod cream*: This immune-response modifier stimulates the body’s immune system to attack and destroy actinic keratosis cells. It is typically applied 2-3 times a week for several weeks. Side effects include redness, itching, burning, and flu-like symptoms, similar to an immune response. The inflammatory reaction is a sign of efficacy and resolution often leaves healthier skin. It is effective for multiple actinic keratosis lesions and provides long-term clearance by leveraging the body’s natural defenses.
3. *Diclofenac gel*: This nonsteroidal anti-inflammatory drug (NSAID) gel is applied twice daily for 2-3 months. It works by reducing inflammation and inhibiting the growth of abnormal cells. It causes milder side effects compared to 5-FU or imiquimod, typically mild redness and irritation. It is particularly useful for patients who cannot tolerate more aggressive topical therapies, though its efficacy might be slightly lower for extensive actinic keratosis.
4. *Tirbanibulin ointment*: A newer topical medication approved for actinic keratosis on the face and scalp. It works by disrupting microtubule function, leading to the death of abnormal cells. Applied once daily for 5 days, it causes localized skin reactions like redness, flaking, and crusting, but often with less severe reactions than 5-FU or imiquimod, and a shorter treatment duration. It’s a convenient option for moderate actinic keratosis burden.
Thirdly, *Photodynamic Therapy (PDT)*: PDT is a field-directed treatment involving the application of a photosensitizing agent (e.g., aminolevulinic acid or methyl aminolevulinate) to the skin, which is absorbed by the actinic keratosis cells. After a few hours, the treated area is exposed to a specific wavelength of light (blue light or red light), which activates the photosensitizer, generating reactive oxygen species that destroy the abnormal cells. The procedure can be uncomfortable during light exposure, causing a stinging or burning sensation. Post-treatment, the skin becomes red, swollen, and crusty, resembling a severe sunburn, for several days to a week. PDT is highly effective for multiple actinic keratosis lesions over a large area, offering excellent cosmetic results and treating subclinical lesions. It is particularly valuable for widespread actinic keratosis on the face and scalp, helping to reduce the overall burden of sun-damaged skin and preventing further progression.
Fourthly, *Curettage and Electrodesiccation*: This lesion-directed procedure involves scraping off the actinic keratosis lesion with a curette (a spoon-shaped instrument) followed by electrodesiccation (burning the base with an electric needle) to destroy any remaining abnormal cells and stop bleeding. It is suitable for thicker, hypertrophic actinic keratosis lesions and is performed under local anesthesia. The treated area forms a scab that heals over 1-3 weeks, potentially leaving a small scar. This method ensures thorough removal of specific, more advanced actinic keratosis lesions that may not respond as well to cryotherapy, offering a definitive treatment for particularly stubborn sun spots. It is often reserved for specific, thicker lesions where a more aggressive removal method is preferred.
Fifthly, *Excision*: Surgical excision involves cutting out the actinic keratosis lesion and a small margin of surrounding healthy skin, followed by suturing the wound. This is typically reserved for actinic keratosis lesions that are suspicious for progression to invasive squamous cell carcinoma, for recurrent lesions, or for larger, indurated lesions where a biopsy and complete removal are desired. Excision provides tissue for histopathological examination, confirming the diagnosis and ensuring complete removal of abnormal cells. The procedure is performed under local anesthesia and leaves a linear scar, making it generally suitable for areas where scarring is less of a cosmetic concern or when malignancy is highly suspected. It offers the highest rate of clearance for the treated lesion and is often the preferred method for any actinic keratosis with features suggestive of early invasion.
Sixthly, *Chemical Peels*: Certain types of chemical peels, particularly those using higher concentrations of trichloroacetic acid (TCA) or Jessner’s solution, can be used to treat widespread actinic keratosis. These peels work by applying a chemical solution to the skin, causing controlled exfoliation and destruction of the superficial layers containing actinic keratosis cells. The skin will peel significantly over several days, revealing smoother, healthier skin underneath. While effective for superficial actinic keratosis and improving overall skin texture, chemical peels are generally less aggressive than 5-FU or PDT and may require multiple sessions. They offer an aesthetic benefit in addition to treating pre-cancerous lesions.
Seventhly, *Laser Resurfacing*: Ablative lasers (e.g., CO2 or Er:YAG lasers) can be used to vaporize the layers of skin containing actinic keratosis cells. This is a highly precise method that can treat large areas and is particularly useful for actinic keratosis on the lips (actinic cheilitis). The recovery period can be significant, with redness, swelling, and crusting lasting several weeks. Laser resurfacing offers excellent cosmetic results and can effectively treat widespread actinic keratosis and severe sun damage, improving the skin’s overall appearance and reducing the risk of skin cancer development. It is often considered for extensive actinic keratosis, especially when other field-directed therapies have been unsuccessful or when cosmetic improvement is a high priority for the patient.
Regular follow-up with a dermatologist is crucial for individuals treated for actinic keratosis, as new lesions can develop over time due to continued sun damage, and a subset of treated lesions may recur or progress. Consistent sun protection, including daily use of broad-spectrum sunscreen, wearing sun-protective clothing, and seeking shade, is paramount in preventing new actinic keratosis lesions and reducing the overall risk of skin cancer. Early detection and prompt treatment of actinic keratosis remain the cornerstone of effective skin cancer prevention strategies.